Key Facts on Health Coverage of Immigrants
On September 17, 2023
Summary
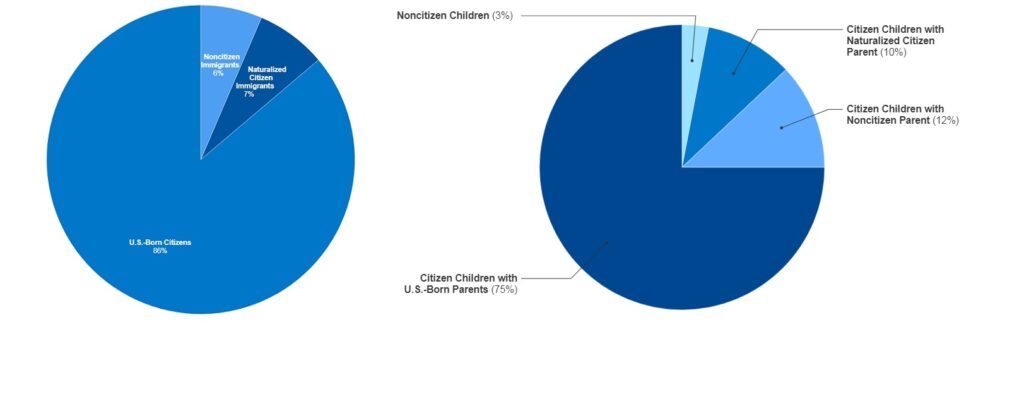
As of 2021, there were 44.7 million immigrants residing in the U.S., including 20.8 million noncitizen immigrants and 23.9 million naturalized citizens, who accounted for about 6% and 7% of the total population, respectively.1 Noncitizens include lawfully present and undocumented immigrants. Many individuals live in mixed immigration status families that may include lawfully present immigrants, undocumented immigrants, and/or citizens. One in four children has an immigrant parent, including over one in ten (12%) who are citizen children with at least one noncitizen parent.2 This fact sheet provides an overview of health coverage for immigrants based on data from The 2023 KFF/LA Times Survey of Immigrants, the largest nationally representative survey focused on immigrants.
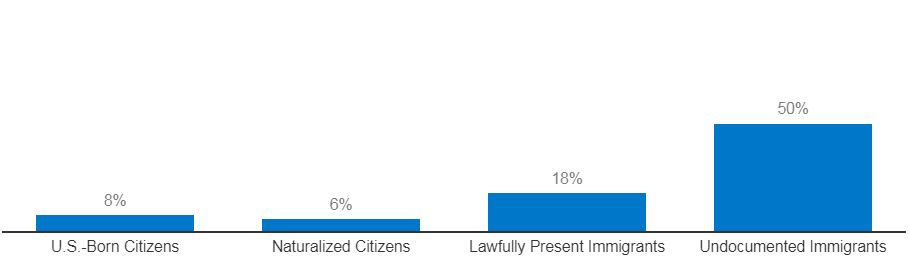
As of 2023, half (50%) of likely undocumented immigrant adults and one in five (18%) lawfully present immigrant adults report being uninsured compared to less than one in ten naturalized citizen (6%) and U.S.-born citizen (8%) adults.3 Noncitizen immigrants are more likely to be uninsured than citizens because they have more limited access to private coverage due to working in jobs that are less likely to provide health benefits and they face eligibility restrictions for federally funded coverage options, including Medicaid, the Children’s Health Insurance Program (CHIP), Affordable Care Act (ACA) Marketplace coverage, and Medicare. Those who are eligible for coverage also face a range of enrollment barriers including fear, confusion about eligibility rules, and language and literacy challenges. Reflecting their higher uninsured rate, noncitizen immigrants are more likely than citizens to report barriers to accessing health care and skipping or postponing care. Immigrants have lower health care expenditures than their U.S.-born counterparts given their more limited access and use.
Some states have expanded access to health coverage for immigrants. At the federal level, legislation has been proposed that would expand eligibility for health coverage for immigrants, though it faces no clear path to passage in Congress. At the state level, there has been continued take up of state options to expand Medicaid and CHIP coverage for lawfully present immigrant children and pregnant people, and a small but growing number of states have expanded fully state-funded coverage to certain groups of low-income people regardless of immigration status. However, many immigrants, particularly those who are undocumented, remain ineligible for coverage options.
Many immigrants remain fearful of accessing assistance programs, including health coverage. The Biden Administration reversed prior Trump Administration changes to public charge rules, which may help reduce fears among immigrant families about participating in non-cash assistance programs, including Medicaid and CHIP. It also increased funding for Navigator programs that provide enrollment assistance to individuals, which is particularly important for helping immigrant families enroll in coverage. However, as of 2023, nearly three-quarters of immigrant adults, including nine in ten of those who are likely undocumented, report uncertainty about how use of non-cash assistance programs may impact immigration status or incorrectly believe use may reduce the chances of getting a green card in the future. About a quarter (27%) of likely undocumented immigrants and nearly one in ten (8%) lawfully present immigrants say they avoided applying for food, housing, or health care assistance in the past year due to immigration-related fears.
Overview of Immigrants
Based on federal survey data, as of 2021, there were 44.7 million immigrants residing in the U.S., including 20.8 million noncitizens and 23.9 million naturalized citizens, who accounted for about 6% and 7% of the total population, respectively (Figure 1).4 About six in ten noncitizens were lawfully present immigrants, such as lawful permanent residents (green card holders) and those with a valid work or student visa, while the remaining four in ten were undocumented immigrants, who may include individuals who entered the country without authorization and individuals who entered the country lawfully and stayed after their visa or status expired.5 Many individuals live in mixed immigration status families that may include lawfully present immigrants, undocumented immigrants, and/or citizens. A total of 19 million or one in four children living in the U.S. had an immigrant parent as of 2021, and the majority of these children were citizens (Figure 1).6 About 9.1 million or 12% were citizen children with at least one noncitizen parent.
Figure 1: Children of Immigrants as a Share of the Total U.S. Population, 2021
Uninsured Rates by Immigration Status
The 2023 KFF/LA Times Survey of Immigrants, the largest nationally representative survey focused on immigrants, provides data on health coverage of immigrant adults and experiences accessing health care, including by immigration status.
Although the majority of uninsured people are citizens, noncitizen immigrants, particularly likely undocumented immigrants, are significantly more likely to report being uninsured than citizens. As of 2023, half (50%) of likely undocumented immigrants and one in five (18%) lawfully present immigrants say they are uninsured compared to 6% of naturalized citizens and 8% of U.S.-born citizens (Figure 2).7
Figure 2 Uninsured Rates among U.S. Adults by Citizenship and Immigration Status, 2023
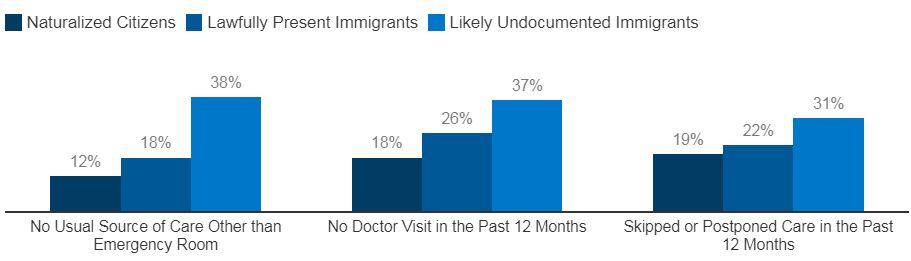
Reflecting their higher uninsured rates, noncitizen immigrants, especially those who are likely undocumented, are more likely than citizens to report barriers to accessing health care and skipping or postponing care. Research shows that having insurance makes a difference in whether and when people access needed care. Those who are uninsured often delay or go without needed care, which can lead to worse health outcomes over the long-term that may ultimately be more complex and expensive to treat. Overall, likely undocumented immigrants are more likely than lawfully present immigrants and naturalized citizens to report not having a usual source of care other than an emergency room, not having a doctor’s visit in the past 12 months, and skipping or postponing care in the past 12 months (Figure 3).8 Lawfully present immigrants also are more likely than naturalized citizens to say they have not had a doctor’s visit in the past 12 months.
Figure 3: Health Care Access and Use among Immigrant Adults by Immigration Status, 2023
Research also shows that immigrants have lower health care expenditures than their U.S.-born counterparts as a result of lower health care access and use, although their out-of-pocket payments tend to be higher due to higher uninsured rates. Recent research further finds that, because immigrants, especially undocumented immigrants, have lower health care use despite contributing billions of dollars in insurance premiums and taxes, they help subsidize the U.S. health care system and offset the costs of care incurred by U.S.-born citizens.
Access to Health Coverage Among Immigrants
Private Coverage
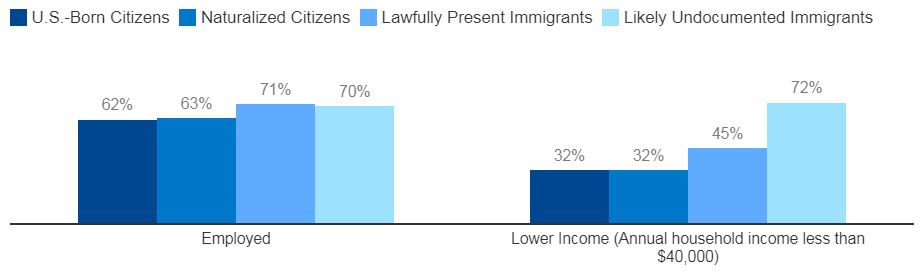
Despite high rates of employment, noncitizen immigrants have limited access to employer-sponsored coverage. Although most noncitizen immigrant adults say they are employed, they are significantly more likely than citizens to report being lower income (household income less than $40,000) (Figure 4).9 This pattern reflects disproportionate employment of noncitizen immigrants in low-wage jobs and industries that are less likely to offer employer-sponsored coverage. Given their lower incomes, noncitizen immigrants also face challenges affording employer-sponsored coverage when it is available or through the individual market.
Figure 4 Employment and Income Among U.S. Adults by Citizenship and Immigration Status, 2023
Federally Funded Coverage
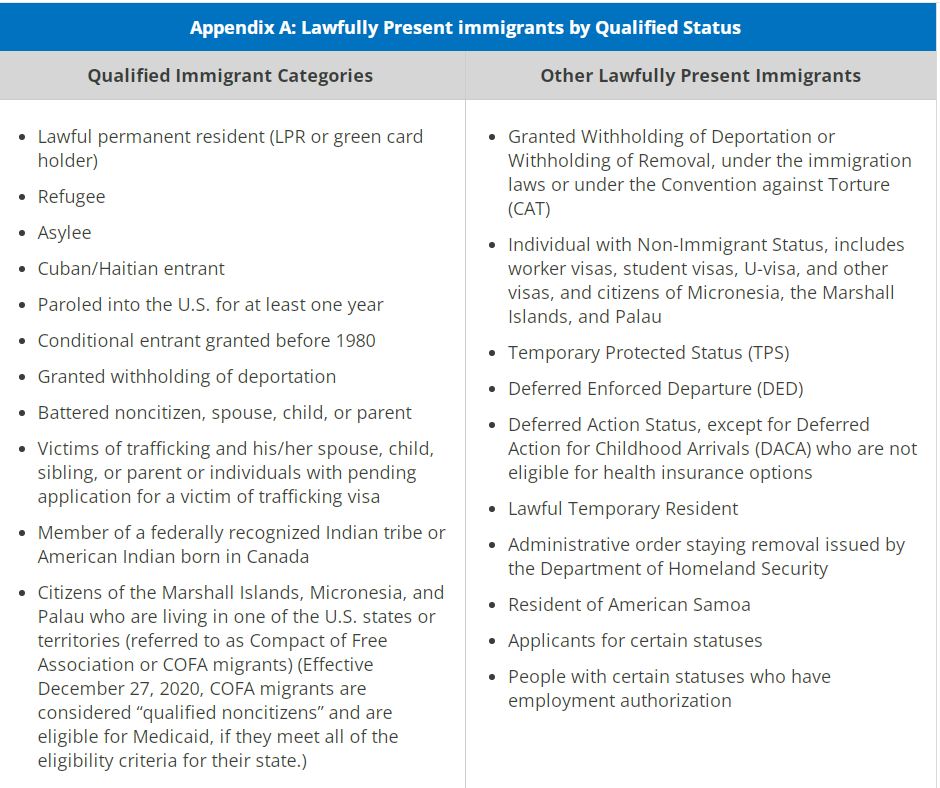
Lawfully present immigrants may qualify for Medicaid and CHIP but are subject to certain eligibility restrictions. In general, lawfully present immigrants must have a “qualified” immigration status to be eligible for Medicaid or CHIP, and many, including most lawful permanent residents or “green card” holders, must wait five years after obtaining qualified status before they may enroll. Some immigrants with qualified status, such as refugees and asylees, do not have to wait five years before enrolling. Some immigrants, such as those with temporary protected status, are lawfully present but do not have a qualified status and are not eligible to enroll in Medicaid or CHIP regardless of their length of time in the country (Appendix A). For children and pregnant people, states can eliminate the five-year wait and extend coverage to lawfully present immigrants without a qualified status. As of January 2023, 35 states have taken up this option for children and 26 states have elected the option for pregnant individuals.
In December 2020, Congress restored Medicaid eligibility for citizens of Compact of Free Association (COFA) communities. The U.S. government has COFA agreements with the Republic of the Marshall Islands, the Federated States of Micronesia, and the Republic of Palau. Certain citizens of these nations can lawfully work, study, and reside in the U.S., but they had been excluded from federally funded Medicaid since 1996, under the Personal Responsibility and Work Opportunity Reconciliation Act. As part of a COVID-relief package, Congress restored Medicaid eligibility for COFA citizens who meet other eligibility requirements for the program effective December 27, 2020.
Since 2002, states have had the option to provide prenatal care to people regardless of immigration status by extending CHIP coverage to the unborn child. As of July 2023, 20 states have adopted this option. (Vermont also offers coverage for pregnant people regardless of immigration status through a state-funded program, see below). Unlike other pregnancy-related coverage in Medicaid and CHIP, the unborn child option does not include postpartum coverage. However, some states that took up this option provide postpartum coverage regardless of immigration status either through a CHIP state plan amendment or using state-only funding. In addition, the American Rescue Plan Act (ARPA) gave states the option to extend Medicaid postpartum coverage from 60 days to 12 months beginning in April 2022. Among the 38 states that have adopted this option, 8 states—California, Connecticut, Illinois, Maryland, Massachusetts, Minnesota, Rhode Island, and Washington—have extended this postpartum coverage to individuals regardless of immigration status using state funds or through a CHIP health services initiative; Colorado will extend it effective 2025.
Lawfully present immigrants can purchase coverage through the ACA Marketplaces and, like citizens, may receive tax credits to help pay for premiums and cost sharing that vary on a sliding scale based on income. Generally, these tax credits are available to people with incomes starting from 100% of the federal poverty level (FPL) who are not eligible for other affordable coverage. In addition, lawfully present immigrants with incomes below 100% FPL may receive tax credits if they are ineligible for Medicaid based on immigration status. This group includes lawfully present immigrants who are not eligible for Medicaid or CHIP because they are in the five-year waiting period or do not have a “qualified” status.
Lawfully present immigrants also can qualify for Medicare subject to certain restrictions. Specifically, they must have sufficient work history to qualify for premium-free Medicare Part A. If they do not have sufficient work history, they may qualify if they are lawful permanent residents and have resided in the U.S. for five years immediately prior to enrolling in Medicare, although they must pay premiums to enroll in Part A.
Undocumented immigrants are not eligible to enroll in federally funded coverage including Medicaid, CHIP, or Medicare or to purchase coverage through the ACA Marketplaces. Under rules issued by the Centers for Medicare and Medicaid Services (CMS), individuals with Deferred Action for Childhood Arrivals status are not considered lawfully present for purposes of health coverage eligibility and remain ineligible for coverage options. On April 26, 2023, the Biden Administration published a proposed rule to expand eligibility for health coverage to DACA recipients. Comments on the proposed rule were due by June 23, 2023, and the final rule is planned to take effect on November 1, 2023, to coincide with the open enrollment period. Medicaid payments for emergency services may be made on behalf of individuals who are otherwise eligible for Medicaid but for their immigration status. These payments cover costs for emergency care for lawfully present immigrants who remain ineligible for Medicaid as well as for undocumented immigrants.
State Funded Coverage
Several states have expanded fully state-funded coverage or subsidies for income-eligible children regardless of immigration status (Figure 5). As of September 2023, 12 states plus D.C. provide comprehensive state-funded coverage to all income-eligible children regardless of immigration status. Colorado currently is using state funds to offer Marketplace coverage with no premium cost for individuals with incomes up to 138% of FPL regardless of immigration status, including children. By 2025, Colorado plans to offer state-funded Medicaid-like coverage to income-eligible children regardless of immigration status. Massachusetts provides primary and preventive services to all children, regardless of immigration status or income. In addition, as noted above, Vermont provides coverage to income eligible pregnant women regardless of immigration status using state-only funds.
Figure 5: State-Funded Coverage for Immigrant Children and Adults, July 2023
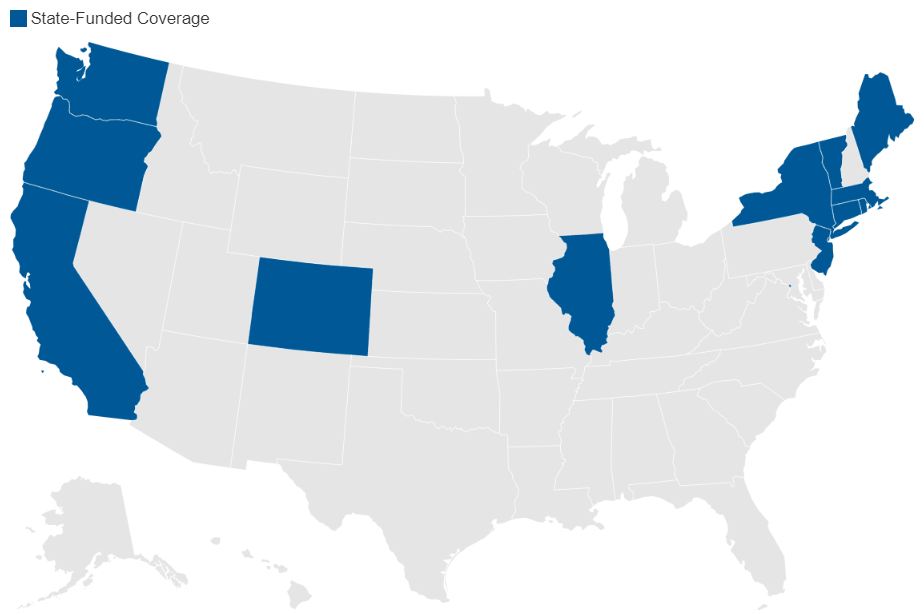
As of September 2023, five states and DC provided state-funded coverage or subsidies to immigrant adults regardless of immigration status. Some additional states cover some income-eligible adults who are not otherwise eligible due to immigration status using state-only funds, but limit coverage to specific groups, such as lawfully present immigrants who are in the five-year waiting period for Medicaid coverage, or provide more limited benefits.
- Through its longstanding locally funded Healthcare Alliance program, DC provides health coverage to low-income residents regardless of immigration status.
- In January 2020, California extended state-funded Medicaid coverage to young adults ages 19-25 regardless of immigration status, and adults ages 50 and older became eligible on May 1, 2022. The state will further extend coverage to income-eligible adults ages 26 to 49 regardless of immigration status no sooner than January 1, 2024.
- In Colorado, beginning in 2023, state residents with incomes up to 300% FPL who do not qualify for health insurance under the ACA or other public programs because of their immigration status are eligible for state-funded premium subsidies to assist them in purchasing individual coverage outside of the ACA Marketplace
- In December 2020, Illinoisextended state-funded coverage to low-income individuals ages 65 and older who were not eligible for Medicaid due to their immigration status. As of July 2022, coverage was also extended to low-income immigrants ages 42 to 64, regardless of status, and proposed legislation would further expand this coverage to all adults ages 19 and older. However, beginning July 2023, Illinois paused enrollment in its Health Benefits for Immigrant Adults (HBIA) program, which covers individuals ages 42 through 64, and placed an enrollment cap of 16,500 for FY2024 on its Health Benefits for Immigrant Seniors (HBIS) program which covers individuals 65 and older.
- In Oregon, the Cover All People Act extended state-funded coverage to all low-income adults who are not eligible due to immigration status, subject to available funding. As of July 1, 2022, coverage was available to those ages 19-25 or 55 and older.
- New York extended state-funded Medicaid coverage to individuals ages 65 and older regardless of immigration status beginning in 2023.
Other states have plans to expand coverage to immigrant adults. In December 2022, CMS approved a State Innovation Waiver from Washington that will allow all state residents regardless of immigration status to enroll in qualified health and dental plans through the state Marketplace and to benefit from state-funded subsidies effective January 1, 2024; the waiver does not affect eligibility for federally funded subsidies. Minnesota will allow individuals regardless of immigration status to enroll in MinnesotaCare, a state-subsidized sliding scale program for low-income residents no sooner than 2025.
Research suggests that state coverage expansions for immigrants can reduce uninsurance rates, increase health care use, and improve health outcomes. California’s 2016 expansion to cover low-income children regardless of immigration status was associated with a 34% decline in uninsurance rates; similarly, a study found that children who reside in states that have expanded coverage to all children regardless of immigration status were less likely to be uninsured, to forgo medical or dental care, and to go without a preventive health visit than children residing in states that have not expanded coverage. Other research has found that expanding Medicaid pregnancy coverage regardless of immigration status was associated with higher rates of prenatal care utilization as well as improved outcomes including increases in average gestation length and birth weight among newborns.
Enrollment Barriers
Among immigrants who are eligible for coverage, many remain uninsured because of a range of enrollment barriers, including fear, confusion about eligibility policies, difficulty navigating the enrollment process, and language and literacy challenges. Research suggests that changes to immigration policy made by the Trump Administration contributed to growing fears among immigrant families about enrolling themselves and/or their children in Medicaid and CHIP even if they were eligible. In particular, changes to the public charge policy likely contributed to decreases in participation in Medicaid among immigrant families and their primarily U.S.-born children. The Biden Administration reversed many of these changes, including the changes to public charge policy, and has increased funding for Navigator programs that provide enrollment assistance to individuals, which is particularly important for helping immigrant families enroll in coverage. However, as of 2023, nearly three-quarters of immigrant adults, including nine in ten of those who are likely undocumented, report uncertainty or an incorrect understanding about how use of non-cash assistance programs may impact immigration status or incorrectly believe use may reduce the chances of getting a green card in the future. About a quarter (27%) of likely undocumented immigrants and nearly one in ten (8%) lawfully present immigrants say they avoided applying for food, housing, or health care assistance in the past year due to immigration-related fears.
Conclusion
Although the majority of immigrants are working, noncitizen immigrants, particularly those who are likely undocumented, have high uninsured rates due to more limited access to both public and private coverage. Federal legislation has been proposed that would expand immigrant eligibility for health coverage, though there is no clear path to passage in Congress. In the absence of federal action, some states are filling gaps in access to coverage for immigrants. However, many remain ineligible for any coverage options, contributing to barriers to access and use of care. Those eligible for coverage also face an array of barriers to enrollment, including fear and confusion about eligibility. The Biden Administration has made changes to public charge policies that are intended to reduce fears of enrolling in health coverage and accessing care and increased funding for outreach and enrollment assistance, which may help eligible immigrant families enroll and stay enrolled in coverage. However, immigrants continue to have significant confusion around public charge rules highlighting the importance of outreach and enrollment assistance, including community-led efforts, to rebuild trust and reduce fears among immigrant families about accessing health coverage and care.
This piece was republished from KFF.