More than 670,000 Texans lose Medicaid coverage as the state unwinds continuous enrollment
By Gloria Farris
On July 20, 2023
Ethel Ruano reapplied for Medicaid coverage in May, something she didn’t have to do for three years.
When officials declared the COVID-19 pandemic a public health emergency in March 2020, initiatives were put into motion to relieve struggling Americans. The Families First Coronavirus Response Act banned states from taking people off Medicaid during the pandemic, regardless of their eligibility status.
Ruano said she earns $360 to $400 each week cleaning houses part-time in Fort Worth. Her family includes her husband and three children. Her youngest, who is 16, was on Medicaid during the pandemic but now he must be reevaluated for coverage.
The enrollments for Texas Medicaid increased by 1.6 million people during the first month of the Act’s operation, an increase of 41%. Three years later, over 5.9 million Texans are enrolled in Medicaid. That’s 2 million more than at the beginning of the pandemic.
Now that the pandemic is no longer considered a public health emergency, eligibility is reverting to what it was before, and states are being forced to remove those no longer eligible.
It is estimated that 50,000 people will lose Medicaid coverage in Dallas County, 15,000 in Denton County, 18,000 in Collin County, and 50,000 in Tarrant County.
“Of course, I am worried. My son has asthma. He needed psychological assistance, too,” Ruano said in Spanish.

Texas began their ‘unwinding’ process in April 2023.
Since then, hundreds of thousands of Texans have been removed from Medicaid.
Ruano has not been told whether she is eligible for coverage. When she first reapplied for Medicaid in May, she said a Texas Health and Human Services representative told her it wouldn’t be until July that she would know if she was eligible.
“Previously, Medicaid or CHIP or any plan that had government budgets would give us 30 business days’ notice,” Ruano said. “And now May, June, July – three months almost. I can be rejected, and it worries me.”
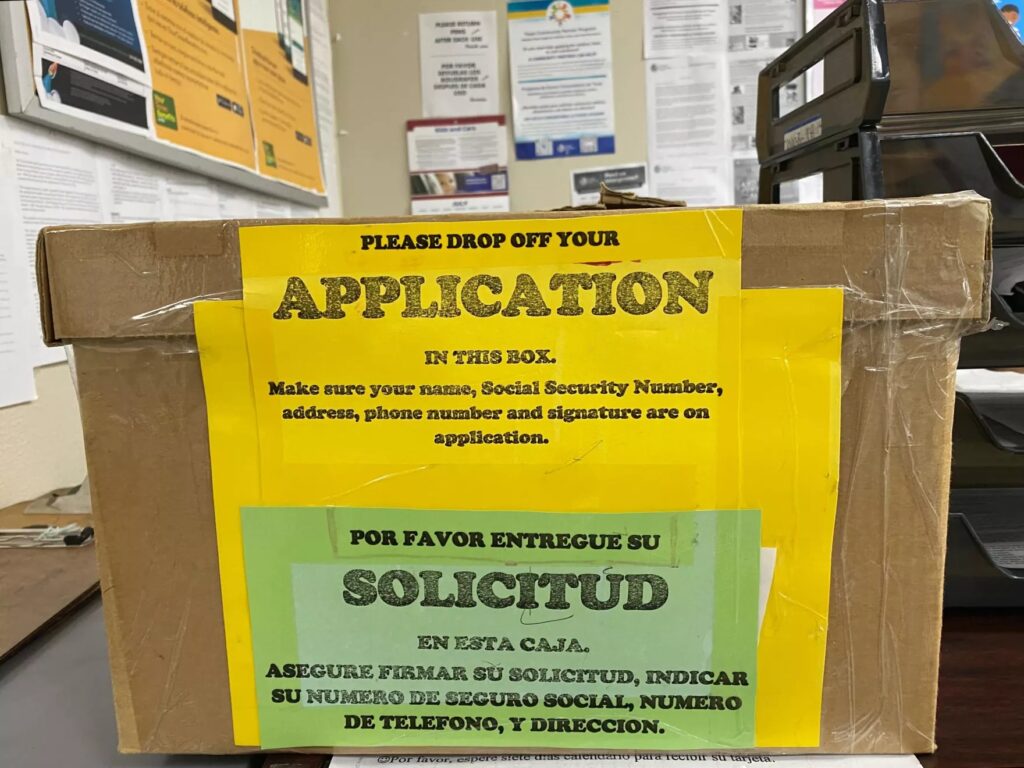
She was grateful to meet Mary Lou Martinez, the outreach and enrollment specialist at North Texas Area Community Health Center (NTACHC) in Fort Worth. Martinez has been helping Ruano with renewing her Medicaid, a burdensome and confusing process for most.
“The parents didn’t have to be renewing (during the pandemic),” Martinez said. “And so, if you had a child during 2020, chances are, you don’t understand about renewing. You didn’t have to do that for three years.”
Who is most at risk?
Texas is required to complete unwinding of ineligible participants by May 2024.
Due to the increased number of cases, the Texas Health and Human Services Commission (HHSC) has hired almost 1,000 employees since April 2022.
Most of the people removed from Medicaid in the past months are ineligible because either they passed the age of 19 during the pandemic, their family’s income increased, or more than two months have passed since they gave birth.
Martinez says most of the patients that they have seen losing Medicaid are young adults who turned 19 during the pandemic.
“We lost them because under normal Medicaid rule, your coverage would end on the month of your 19th birthday,” she said. “And when it (the pandemic) happened, they continued to have coverage for three years so now they will not qualify for Medicaid again.”
She said that there are a few that will qualify if they are full-time students and do not have a job.
According to new data, 81% of Medicaid denials so far have been due to procedural reasons.
Diana Forester, director of health policy at Texans Care For Children, said in a press release that this number of procedural denials should be setting off alarm bells.
“When you see this many procedural denials, it means that the process is not working properly, whether the state is sending renewal information to the wrong mailing addresses or parents are running into bureaucratic delays with the state when they try to renew their children’s health insurance,” Forester said.
Qualifying for Medicaid coverage
Dr. Patricia Rodriguez is a health care provider at NTACHC. Her patients have been affected by the Medicaid unwinding.
“I think the biggest concern as a pediatrician is that I may not be able to see some of the patients that were previously insured,” she said. “And I get concerned that some of those kids might go without care because of that coverage.”
Those who do not qualify for Medicaid may qualify for other programs like Children’s Health Insurance Program (CHIP) or Affordable Care Act’s individual Marketplace.

Those who don’t qualify for any federal benefits and are uninsured now may turn to federally funded clinics like NTACHC.
Rodriguez says that their clinic will see patients regardless of insurance status.
“That’s what makes us different than a normal or typical health center provider,” she said. “We are special in that way because of our federally qualified status.”
That’s why Ruano is not more worried about her Medicaid application.
“If Medicaid turns me down, I know I have options with them here,” she said.
Still, the HHSC recommends that anyone with Medicaid insurance stay up to date on their renewal status by registering an account on YourTexasBenefits.com or contacting HHSC with any questions by calling 2-1-1 or 877-541-7905.
The HHSC website also encourages Medicaid users to report any changes in their profile like their address or phone number to the Commission through the website or telephone number so their coverage doesn’t change unexpectedly.
Lucia J. Weatherall used to be enrolled in Medicaid before she started working for Texas HHSC as a field policy services manager. Now she helps people enroll in Medicaid and understand their health benefits.
“Everybody might need help,” she said. “It’s just you don’t know their business, but everyone might need assistance. So, you always treat somebody like that’s your mom and you always want to make sure that you provide them what they need.”
This piece was republished from KERA PBS News.