Race, Maternal Age, and Social Vulnerability Affect Risk of Severe Maternal Morbidity
By Franklin B, Piff A, Bartelt K, Joyce B, and Tang D
On November 28, 2023
Key Findings
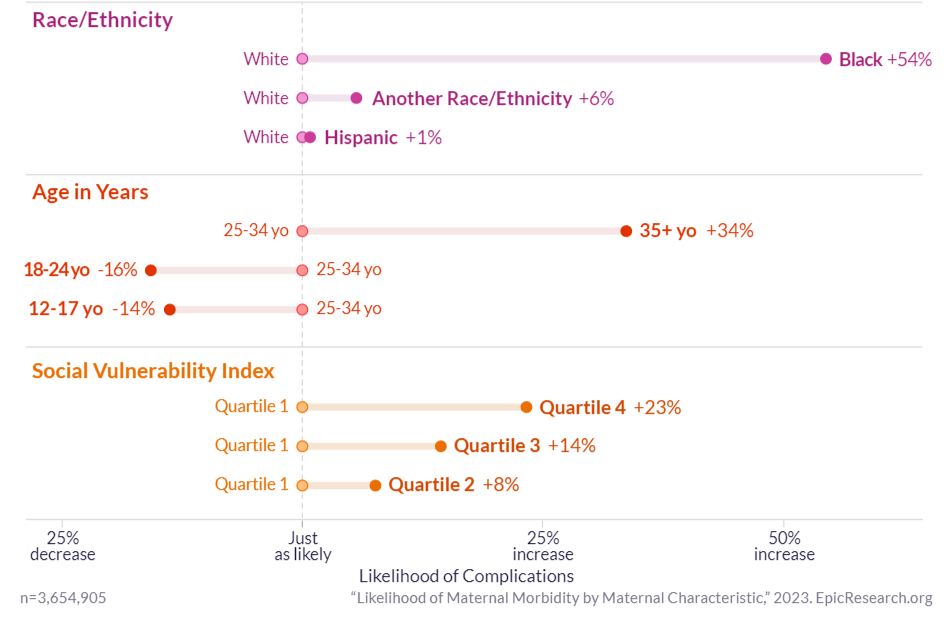
- Women who are Black, aged 35 or older, or in the highest social vulnerability index (SVI) quartile have greater odds of being diagnosed with a severe maternal morbidity (SMM) condition than women who are White, 25-35 years old, or in the lowest SVI quartile, respectively.
- Black race has a stronger correlation with a SMM condition diagnosis than any other factors studied, including maternal age or SVI.
Severe maternal morbidity (SMM) is a group of complications that occur during pregnancy or delivery and that have an impact on a woman’s health, such as embolism, sepsis, and acute renal failure. The Centers for Disease Control and Prevention (CDC) reported that these complications have been on the rise.1 Because these complications can have lasting impacts, Healthy People 2030, an initiative set forth by the U.S. Department of Health and Human Services (HHS), aims to reduce rates of SMM, as well as disparities in the incidence of SMM by race and ethnicity.2 Previous studies have found that women of color and those with advanced age were associated with higher odds of SMM.3,4
To understand whether race/ethnicity, maternal age, or social vulnerability index (SVI) is most correlated with an SMM condition diagnosis, we evaluated 3,654,905 pregnant women between January 1, 2017, and June 30, 2023, for maternal morbidity outcomes. After controlling for other potential factors, such as age and SVI, we found that Black women have 54% greater odds of being diagnosed with an SMM condition than White women. Other non-Hispanic women have 6% greater odds and Hispanic women have 1% greater odds than White women. Women aged 35 and over have 34% greater odds of being diagnosed than women aged 25-34. Those aged 12 to 18 have 14% decreased odds and those aged 18 to 25 have 16% decreased odds. Finally, women in the most vulnerable SVI quartile (quartile 4) have 23% greater odds of being diagnosed with an SMM condition than women in the least vulnerable quartile (quartile 1), while those in quartile 3 have 14% greater odds, and those in quartile 2 have 8% greater odds.
FIGURE 1
Likelihood of Maternal Morbidity by Maternal Characteristic
A sensitivity analysis using Area Deprivation Index (ADI) instead of SVI to assess the degree to which a patient’s environment might affect their vulnerability also found that women who are Black, women who are over age 35, or who are in the most vulnerable ADI quartiles are at the highest risk of SMM diagnosis. Race remained the most correlated variable across both analyses. This racial disparity may be reduced through improved hospital quality, standardization of care, and timely recognition and response to acute illness.5
This piece was republished from Epic Research.