Researcher brings addiction-care ‘hubs’ to Capitol Hill
Q&A: Caleb Banta-Green of UW Medicine discusses an approach to reduce overdose deaths, now part of a bill in Congress. June 25, 2024
Media Contact: Brian Donohue – [email protected], 206-543-7856

Last month, two U.S. senators introduced bipartisan legislation called the Fatal Overdose Reduction Act. The bill aims to reduce the outsize, deadly impact of fentanyl and other illicit opioids on American communities.
One aspect is the creation of Health Engagement Hubs, a care model co-developed by Caleb Banta-Green, research professor in psychiatry and behavioral sciences at the University of Washington the School of Medicine. The hubs are the latest iteration of a care approach that began in 2015 and involved input from community-based agencies and local and state government partners.
In a Q&A, Banta-Green discussed fentanyl and why he thinks the hub care model holds promise. The Q&A has been edited for length and clarity.

Q: Fentanyl’s growth as a public health threat has been sharp and striking. Was this drug on addiction specialists’ radar 10 years ago?
Banta-Green: We’d heard about fentanyl in Detroit around 2006, with connection to a manufacturing lab in Mexico. So we knew the potential for illicit fentanyl to come into the market. But then it was quiet for several years before it hit here in Washington state around 2016, and really took off around 2020. By 2022, we were seeing far more fentanyl than we ever saw with heroin.
Q: In your circle, did any researchers imagine it would be a problem at the scale it is today?
Banta-Green: We’d seen heroin for many years. Then we saw pharmaceutical opioids, and then this (fentanyl) just surpassed both of those by more than 150% in just a few years. We just had no reason to ever think we’d see that level of opioid overdoses.
Q: How is fentanyl different from heroin?
Banta-Green: Fentanyl is about 50 times more potent than heroin, and it’s faster acting and it’s shorter acting. So for heroin, you might see the drug come on, have a peak effect and go down over four or six hours. With fentanyl, you might see all that in 20 minutes. And if a person becomes dependent, they have to use over and over again to feel well. So fentanyl’s overdose risk is very high.
It’s an easier drug to use because it can be used in a pill or smokable form as opposed to injection like heroin, so the barrier to entry is much lower. An adolescent is more likely to use fentanyl than they would’ve been to use heroin.

Q: How do other illicit drugs line up against fentanyl in terms of use and overdose?
Banta-Green: Methamphetamine deaths are right (below fentanyl). If it weren’t for fentanyl, we’d be talking about meth. We just completed the statewide syringe-services program survey. Among folks who said their primary drug was fentanyl, 85% also reported using methamphetamine. So the overlap is profound, and that’s important to understand because it has implications for how people are behaving and what treatments and supports they need to move into recovery.
Q: What has fentanyl taught you about drug addiction?
Banta-Green: Fentanyl has taught us how high a person’s tolerance can be on an opioid, which we never knew. We know that, as people use opioids, they (develop) more tolerance. People are using (fentanyl) much more often, so we have to use our treatment medications in new ways to match that level of tolerance — ways that my medicine colleagues are stunned by, but have learned to treat successfully.
Q: What’s an easy way to understand health-engagement hubs?
Banta-Green: The idea is that you’re bringing a lot of different services together: opioid-use disorder treatment, physical healthcare, some mental healthcare, as well as infectious-disease prevention and overdose prevention. It’s bringing all of that into a one-stop shop.
Q: Why would people who have a drug addiction problem want to go to a hub?
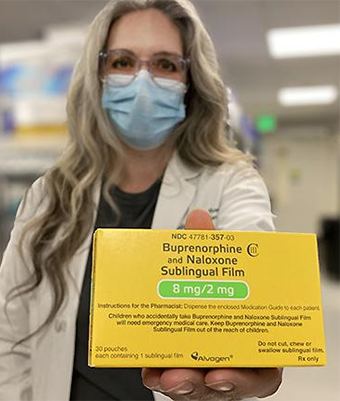
Banta-Green: The reasons are twofold: One is that basically everybody who’s using fentanyl wants harm-reduction services. They don’t want to get HIV, they don’t want to get hepatitis, they don’t want overdoses, so they want harm-reduction services and supplies. Second, the vast majority of people also want to stop their use, and they know that the treatment medications buprenorphine and methadone are the most effective way to do that. So by bringing those things together, we have something for everybody every day, whether they want to stop using or whether they just don’t want to die that day.
We’re creating an environment where people are treated well (and) where staff have the expertise and time to engage with people. And then the services: harm-reduction services, overdose prevention materials, infectious-disease prevention materials and supplies, as well as the treatment medications, buprenorphine and methadone, which rapidly treat opioid-use disorder.
Q: How did this model of care become a bill in Congress?
Banta-Green: The bill in Congress is a long path of over 10 years of research and partnership with community agencies to try new approaches — and, as a researcher, testing and evaluating them and seeing what the right mix of services and care are.
And as we’ve done that, we’ve repeatedly shown positive outcomes, specifically with really marginalized folks who are now accessing services they’ve been unable to in other care settings. We’ve seen substantial reductions in illicit opioid use and significant reductions in mortality.
In that process, I also work with and educate the Washington State Legislature. We’ve developed recommendations that have become legislation. So then when our federal partners reached out and said, “What can we do?” we were able to point to the work that we’ve already done in Washington State and say, let’s try this nationally.
Q: In your testimony on Capitol Hill, you mentioned that the process of breaking free of addiction takes time. Can you talk about that?
Banta-Green: Recovery is not binary, linear or short. It is a process, and so we need to help people through that process.
What we found with the low-barrier buprenorphine clinic we started in 2017 in downtown Seattle was people had very different patterns. Some people would come in on Day 1 and stay on care. Some people would come on Day 1 and never come back. But oftentimes people would come in for a couple of weeks, they’d disappear, come back for a couple of weeks, come back, and then it would stick.
I also did an analysis of the state prescription-monitoring program data for all of the buprenorphine in the state, and we found the same thing: It might be the first, second, third or fourth try starting medications before a person had long sustained time on medication and long sustained recovery. It’s about never giving up on people, and it’s the reason behind health engagement hubs not just being a place where people can drop in any time, but keep coming back no matter what.
Q: How do you respond to the argument that, by providing supplies for smoking and injecting drugs, these hubs are contributing to illicit drug use?
Banta-Green: Our goal is engagement. Our goal is for people to come in and to keep coming back, and that means offering them something that benefits them and their health that day. And so that may be providing them education and materials that keep them from overdosing or getting hepatitis or HIV, those harm-reduction materials. That may be what brings them in that day. It might be that they want treatment medications. It might be that they desperately need wound care. So we want to offer whatever they need that day that will bring them in and keep them safe that day. And hopefully they’ll engage in things that keep them safe over the long term, as well.
Q: What do you think the prospects are of this bill passing?
Banta-Green: I’m cautiously optimistic. I think it’s difficult to get a bill like this passed on the first round. I think it is a bipartisan issue. What can take some time is everyone recognizing that nobody deserves to die.