The Aging Prison Population: Causes, Costs, and Consequences
By Emily Widra, August 2, 2023
New Census Bureau data show the U.S. population is getting older — and at the same time, our prison populations are aging even faster. In this briefing, we examine the inhumane, costly, and counterproductive practice of locking up older adults.
New data from the Census Bureau reveals that the U.S. median age rose to a high of 38.9 years: an increase of three and half years in the last 23 years. The U.S. prison population is aging, too, and at a much faster rate than the nation as a whole — and older adults represent a growing portion of people who are arrested and incarcerated each year. The aging of the prison population is the result of a series of disastrous policy decisions in policing, sentencing, and reentry over roughly the last half-century. And while prisons and jails are unhealthy for people of all ages, older adults’ interactions with these systems are particularly dangerous, if not outright deadly.
Aging throughout the criminal legal system
Older adults are increasingly ensnared in all parts of the criminal legal process: in arrests, pretrial detention, and imprisonment. In 2000, 3% of all adult arrests involved people aged 55 or older, and by 2021, this older population accounted for 8% of all adult arrests. According to the most recent available data on local jails across the U.S., from 2020 to 2021 — during the COVID-19 pandemic, which was particularly dangerous for older adults — the segment of the jail population aged 55 and older expanded by a greater proportion than any other age group, growing 24% compared to an average increase of 15% across all other age groups.
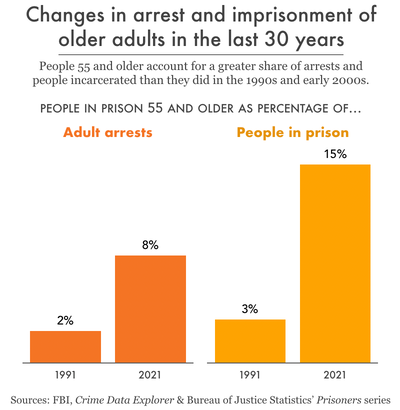
Meanwhile, older people make up five times as much of the prison population as they did three decades ago. From 1991 to 2021, the percentage of the state and federal prison population nationwide aged 55 or older swelled from 3% to a whopping 15%. This growth is seen even more acutely when looking at people serving life sentences: by 2020, 30% of people serving life sentences were at least 55 years old, with more than 61,400 older adults sentenced to die in prison.
The dangers of aging in prison
Prisons are unhealthy places for anyone of any age, but keeping older adults locked up is particularly dangerous. A robust body of research shows that incarceration itself accelerates aging: people face more chronic and life-threatening illnesses earlier than we would expect outside of prison, and physiological signs of aging occur in people younger than expected. In addition, a conservative estimate of more than 44,000 people 45 and older experience solitary confinement in state prisons each year, in conditions that shorten lives and can be detrimental to physical, mental, and emotional health. Years of limited resources, inaccessibility, and understaffing in prison healthcare have created a situation in which each year spent in prison takes two years off of an individual’s life expectancy. The same scarcity of prison healthcare resources that jeopardizes older people’s health is not just ineffective-it’s also exorbitantly expensive.
The high costs of incarcerating older people
State and federal governments spend increasingly more money on consistently inadequate healthcare for their growing populations of older adults. While most studies on the steep costs of incarcerating older people date back at least a decade, their findings are consistently dramatic. For example, in California prisons in the 1990s, the state spent three times as much money to incarcerate an older person than someone of any other age group. Considering the proportion of California’s prison population over the age of 50 has risen from about 4% in 1994 to 25% in 2019, and that prison healthcare spending per-person has ballooned in the intervening years, the cost of incarcerating older adults only appears to be growing. In 2013, the federal Bureau of Prisons (BOP) spent 19% of its total budget — or $881 million — to incarcerate older adults. That same year, the BOP reported this group was the “fastest growing segment of its inmate population” with a 25% increase over the course of a single year (as the rest of the population decreased by 1%).
As long as people are in prison, they should receive the care they need to be safe and healthy. But especially at the state and local level, every dollar spent in prisons is a dollar that could have expanded and improved community health services — and provided superior care. It doesn’t make much sense to spend so much money locking people up in places that are not only dangerous to their health, but more costly to care for them — especially when there is little public safety argument to justify doing so.
Low risk of re-arrest and re-incarceration for older adults
The older someone is, the less likely they are to be arrested following release from prison, according to the most recent government study of recidivism. In fact, people released at age 65 or older are the least likely of any age group to be re-arrested in the five years following release:
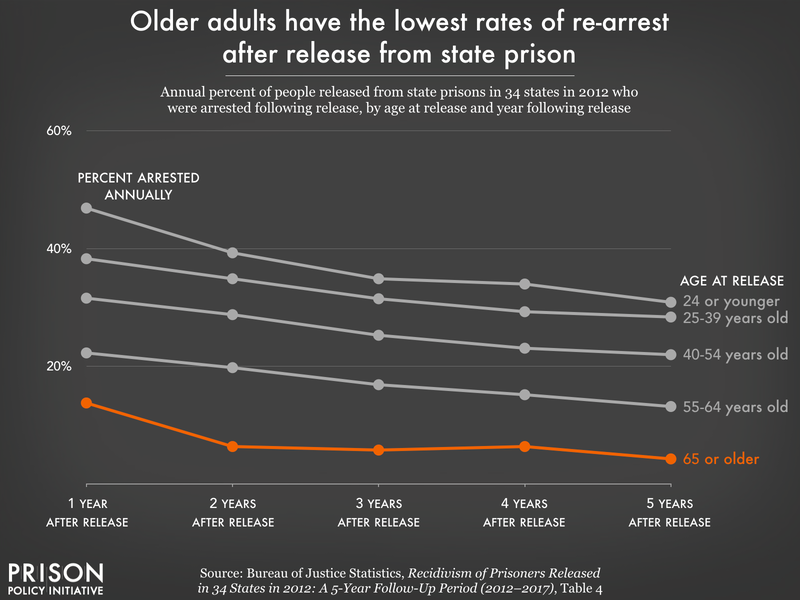
Decades of research reinforces these findings: formerly incarcerated older adults are among the least likely to be re-arrested, re-convicted, and reincarcerated.
Decades of “tough on crime” policies contributed to the aging prison population
The incarcerated prison population is getting older much more quickly than the general population because of policy choices throughout the criminal legal system.
Policing
Policing disproportionately targets populations that often include many older adults: unhoused people, people who use drugs or alcohol, and people with cognitive disabilities. Nationally, the unhoused population is growing older. From 2007 to 2014, the number of unhoused people over age 50 expanded by 20%, and in 2014, this age group accounted for more than 30% of people experiencing homelessness. Given that unhoused people are up to 11 times more likely to be arrested than housed people, the likelihood of arrest for older, unhoused people is undoubtedly growing over time. Drug-related arrests among people aged 50 and older nearly doubled from 2000 to 2018, indicating a dramatic increase in criminal legal system involvement.
The criminalization of mental illness among older adults is significant as well. One in nine people aged 65 and older have Alzheimer’s dementia (one of many kinds of dementia). The most recent national data available indicates that people with cognitive disabilities are overrepresented in jails and prisons: 31% of people in jails in 2012 and 24% of people in state prisons in 2016 reported a cognitive disability. As greater numbers of older adults with cognitive disabilities encounter police, older prison populations are likely to grow.
Sentencing
State and federal sentencing policies from the 1970s to the 2000s resulted in what researchers have called “a prescription for an increase in older inmates: more prisoners, more prison beds, more lifers, and less parole.” State and federal laws enacted in this time period resulted in more incarcerated people serving longer sentences via policies that:
- Increased sentence lengths and established mandatory minimums,
- Mandated extremely long sentences for individuals convicted of three felony offenses (“three strikes” laws),
- Required people to serve upwards of 85% of their sentence in prison (“truth in sentencing” laws) before becoming parole eligible,
- Abolished parole,
- Reduced the allowed time earned for good conduct, and
- Instituted other “tough on crime” sentencing laws.
Longer and harsher sentences top the list of the most obvious mechanisms by which the national prison population exploded in the 1990s and 2000s, but they also created the problem of today’s aging prison population: many of the people who received these sentences are still behind bars now that they are twenty or thirty years older.
Tools to reduce the aging prison population remain underutilized
While attention to this crisis has grown in recent years, many of the available tools — such as parole and compassionate release — have been underutilized. The failure to release older adults from prison has deadly repercussions: from 2001 to 2018, over 30,500 people aged 55 or older died in prison and almost all of these deaths (97%) were due to illnesses.
Parole
In a study of parole in Maryland, the Justice Policy Institute found that between 2017 and 2021, parole grant rates are highest for people between the ages of 31 and 35 (43%) with rates declining as age increases: people over 60 are paroled at a rate of 28%. Older adults serving long sentences are often denied parole, with boards focusing on the nature of their original offense instead of their preparedness for reentry. That being said, parole is not even an option for large swaths of the prison population. Almost half of all people serving life without parole (LWOP) sentences are at least 50 years old, and one in four is at least 60 years old. Even some “geriatric” or “elder” parole laws, intended to facilitate the release of older incarcerated people, needlessly exclude many older people who would otherwise be eligible; for example, the Justice Policy Institute points out that the Maryland law only applies to older people with multiple convictions.
Compassionate release
Compassionate release (often called medical parole) is an important release mechanism for older adults, but is not used nearly often enough. The application process is cumbersome and opaque, and many people die before they ever receive a decision. In addition, decisions about medical eligibility for release are often filtered through state parole boards, whose membership often includes former corrections officials, former parole or probation officers, and former prosecutors. These are not vocations particularly invested in release, much less promoting individual health and wellbeing outside of the carceral system. Parole boards’ lack of knowledge about serious and terminal illnesses, as well as the general aging process, can create significant barriers to release. Physician reluctance to offer a prognosis, parole board rejections of medical recommendations, offense carveouts, and barriers to discharge planning also factor into the underutilization of compassionate release. Some states (like Iowa) do not even have such a release program.
The result: Nursing homes behind bars
As a result of the disastrous failure to make use of existing release systems and increasing public pressure to address the aging prison population, prisons have adapted in very troubling ways. In Connecticut, Kentucky, Tennessee, and Wisconsin, departments of corrections have created “prison nursing homes” to keep people incarcerated even when they are far too sick or frail to represent any kind of public safety threat. The continued incarceration of people who would otherwise be receiving residential or long-term care reflects a troubling trend of prisons “gearing up to become nursing homes, but without the proper trained staff and adequate financial support.”
Re-entry barriers
Many people released from prison — regardless of age — struggle to obtain adequate and affordable housing, employment, and healthcare. For older adults, these concerns can be magnified as any amount of time spent in prison disrupts healthcare services and increases the challenges of (re)connecting with them after release. Older adults also have fewer relationships with people on the outside, face discrimination in healthcare settings like nursing homes, and come up against legal and regulatory barriers to accessing benefits like Supplemental Security Income and Medicare.
The sheer number of complex and overlapping barriers placed before formerly incarcerated older people is staggering:
Barriers to admission for nursing homes and other necessary healthcare facilities are particularly awful for people who have a terminal illness and are released via compassionate release. In Connecticut, many nursing homes will not even consider admitting people released from prison, and in Florida, people who have been convicted of sex offenses and released from prison often live in motels because they are routinely turned away from nursing homes. Formerly incarcerated older adults facing chronic and terminal illnesses are often forced to rely on an “ad hoc network of care” for their medical needs.
Reducing the aging prison population
If we hope to address this crisis, more work needs to be done to curb arrests of older people, to divert them to better community support, and to reduce their numbers behind bars. The decriminalization of homelessness and substance use — as well as expanded diversion services for older adults — can reduce their risk of arrest and detention. States can also send fewer people back to prison by eliminating parole revocations for technical offenses that reincarcerate people for actions that, were the individual not on parole, would not be crimes at all.
To reduce the number of already-incarcerated older adults, state and federal governments can make use of presumptive parole, second-look sentencing, and the retroactive application of sentence reduction reforms, as well as the many other mechanisms to shorten excessive prison sentences outlined in our 2018 report, Eight Keys to Mercy: How to shorten excessive prison sentences. All states should have compassionate release or medical parole available to release older adults and those facing chronic and terminal illnesses. States can also reduce existing barriers to compassionate release by eliminating exclusions based on offense type, relaxing eligibility criteria, and simplifying the application, review, and approval process. Elder parole policies that implement automatic parole consideration for older adults who have already served some portion of their sentence can further reduce the number of older people behind bars, simplifying the process of getting out of prison for some of the most medically vulnerable people.
Finally, states and the federal government need to expand the social safety net to support older adults released from prison. There are numerous interventions to support reentry by reducing housing and employment barriers, encouraging access to healthcare and health insurance (including Medicare and Medicaid), and simplifying application and re-enrollment for Social Security benefits, as well as many more crucial supports outlined in this 2022 issue brief from Justice in Aging.
Conclusion
The crisis of our aging prison population is not an accident but the result of policy choices that hurt incarcerated people, their loved ones, families, and communities. Fortunately, we can address these policy missteps.
In order to provide older incarcerated people with adequate healthcare, end of life care, and dignity, we need to find ways to reduce their numbers in all parts of the carceral system. Existing tools — like compassionate release and parole — can help but are not enough to address this problem on their own. States should follow the lead of advocates who are fighting to reduce police encounters, end draconian sentencing like life without parole, and expand release mechanisms like elder parole. Reducing barriers to enrollment in Medicare, Medicaid, Social Security, and ensuring people have safe places to live in our communities can expand the safety net for older adults leaving prisons. Ultimately, the benefits of such changes will not be recognized only by older adults in the system but the broader population as well.
This article was originally published on August 2nd, by the Prison Policy Initiative.